Prostate Information
Overview
As men age (particularly after the age of 40), they are more susceptible to prostate problems. Prostate glands never stop growing, however this growth does not typically pose a problem until an advanced stage. More than 50% of men who have reached the age of 60, and up to 90% of men who have reached the age of 80, experience symptoms of an enlarged prostate.
Prostate problems for most men are an embarrassing topic of conversation, as there are both sexual issues and complications with urination. Even so, having an enlarged prostate is not unusual. As men continue to live longer, having an enlarged prostate is becoming more common. In the year 2000, in the United States, there were 4.5 million appointments made with doctors to address enlarged prostates. The numbers are staggering.
About the Prostate
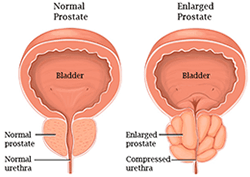
Located just below the bladder, the prostate is a small exocrine gland (about the size of a walnut) that is part of the male reproductive system, which sits directly next to the seminal vesicles and consists of two lobes that are encased in tissue. The prostate produces a milky white alkaline fluid that nourishes and protects sperm cells. The urethra, a tube that carries urine and semen to the penis, runs directly through the prostate. The fluid that is produced by the prostate mobilizes the sperm and plays an important role in reproduction. The prostate grows and develops by stimulation from sex hormones called androgens; the main androgen hormone is testosterone which is produced by the testicles.
That said, it is unknown exactly, what all the functions of the prostate actually are.
Prostate Health
Prostate health is a major concern for millions of aging men. The prostate is an integral part of the male reproductive system that deteriorates as men age leading to various forms of issues and discomfort. However, prostate issues and discomfort are not just for “old men” as is the popular misconception. Prostate health should be of interest for every man over the age of 40. Unfortunately, more and more men in their 30’s are also facing prostate issues, this is primarily due to diet and lifestyle choices which have an enormous impact on their health. These issues include: BPH (Benign Prostatic HyperPlasia or Hypertrophy), also known as an Enlarged Prostate and Prostatitis, which manifests in many forms, and can lead to chronic pain.
BPH (Benign Prostatic HyperPlasia or Hypertrophy)
BPH (Benign Prostatic HyperPlasia or Hypertrophy) is the medical term for the condition known as an Enlarged Prostate
Prostate growth affects virtually all men over 50. Symptoms of difficult urination tend to increase with age. Medicines or surgery can address BPH. As males age, there are two times when the prostate grows. The prostate may grow to twice its previous size when males enter puberty. Then when males reach the approximate age of 25, the prostate begins to grow once more. This second growth phase can result in greater prostate issues down the road.
When the prostate grows, the tissue that encases the gland keeps it from expanding, which means that the prostate begins to put pressure on the urethra. This, in turn, leads to thicker bladder walls. The bladder then starts to contract, regardless of the amount of urine contained in it. This contraction leads to an increased urgency to urinate. Over time, the bladder becomes weaker and is unable to fully empty during urination. The pressure on the urethra and the inability to fully empty the bladder can lead to further complications of the enlarged prostate.*
Prostatitis
Prostatitis is inflammation of the prostate, sometimes caused by infection. In some cases, antibiotics can help.* There is no age limit and it strikes men young and old alike; and may lead to lifelong distress if not dealt with properly.
There are many forms of prostatitis but the two most common are bacterial and non-bacterial. As it sounds, bacterial prostatitis is caused by bacteria invading the prostate (usually E. coli) which may result in infection and inflammation.* Non-bacterial prostatitis (or CPPS – Chronic Pelvic Pain Syndrome) is often caused by stress and other lifestyle factors but the true cause is unknown. Both of these forms of prostatitis have significant sexual and urinary symptoms including painful ejaculations and acute pain in the pelvic region.
Causes and Symptoms of Prostate Issues

Medical experts are currently unable to isolate the definite causes of most prostate issues. As such, the risk factors are largely unknown. However, it is known that age, genetics and lifestyle choices (exercise and diet) all play contributing roles.
There are many different symptoms, depending on the condition, but the main ones are related to issues with urination. These include:
- Nighttime trips to the toilet
- Weak stream when passing urine
- Frequent and sudden urges to urinate
- Dribbling after urination
- Incomplete voiding of bladder after urination
- Blood in the urine or semen
- Painful or burning urination
- Difficulty starting urination
- Trouble getting an erection
- Weakness or numbness in the legs or feet
Diagnosis and Management
There are numerous tests that can assist an urologist (a doctor who specializes in conditions related to the male reproductive system and urinary tract) in the diagnosis of prostate related issues. Not every male will require every test, but here is a list of the most prevalent ones:
- Digital Rectal Exam (DRE) – This will most likely be the first test administered. The doctor will insert a lubricated gloved finger inside the rectum to palpate the prostate. This procedure will allow the doctor to determine how big the prostate is.
- Prostate Specific Antigen (PSA) Blood Test – PSA is a protein that is created by prostate cells which can be measured by a blood test. If high PSA levels are detected, an enlarged prostate is the most likely cause.
- Transrectal Ultrasound – In this type of ultrasound, a probe is inserted inside the rectum to send sound waves to the prostate. These waves create an echo that allows a picture of the gland to show up on a monitor. This ultrasound is often done with a biopsy to test for prostate pathogens.
- Urine Flow Study – Doctors will perform this test to determine the rate of urine. Males urinate into a specially designed container and if the flow is slow or hesitant, it could serve to diagnose BPH.
- Cystoscopy – This procedure requires the insertion of a tube into the urethra through the penis. The tube is known as a cystoscope and is made up of a light and a lens that allow the doctor to view the bladder and urethra. The doctor can then see the size of the prostate and find out how much of the urethra is obstructed.
- Prostate Biopsy – A needle is inserted through the rectum and into the prostate to excrete tissue in order to check for prostate pathogens.
Appropriate management depends on the severity and type of condition experienced.
Natural Alternatives
All in all, this is really quite distressing news for men. None of these render pleasant images, and of course none of them are very comfortable even so far as to say, traumatizing.
Supporting a healthy prostate, before issues occur, is perhaps the most important way forward, avoiding potential problems that may occur as men age. Nourishing the prostate gland to ensure healthy function, through a healthy diet and regular exercise is a great start. Natural supplements formulated to target mineral and vitamin deficiencies may, as well as, help balance hormones.*
Even after a diagnosis, nourishing support may help minimize symptoms and help manage an enlarged prostate gland by reducing inflammation. Either way, a quality supplement may provide the support to bring much needed relief.*
To better understand what to look out for when choosing a prostate supplement, click on “Choosing A Product”. Alternatively, click on “Product Comparisons” to discover which supplements we felt may provide your body with all that it might need to overcome the many challenges that an unhealthy prostate can bring.
